Managing Stress Urinary Incontinence: Modern Robotic Solutions and Practical Tips
Urinary incontinence affects one in three women at some point in their lives, yet many suffer in silence for far too long. The good news? It's highly treatable, and today's options are more sophisticated than ever.
This guide breaks down what you need to know about stress urinary incontinence, from lifestyle changes to cutting-edge robotic surgery.
Understanding the Different Types of Incontinence
Not all leakage is the same, and treatment depends on getting the type right:
Stress Urinary Incontinence
Leakage when coughing, laughing, lifting, or exercising
Usually linked to weakened pelvic floor support
Urgency Incontinence
Sudden, overwhelming need to urinate
Often includes frequent trips and nighttime urgency
Caused by overactive bladder muscles
Mixed Incontinence
Combination of stress and urgency symptoms
Other Types
Overflow or functional causes (less common)
Usually related to neurological conditions
Why It Happens
Several factors can trigger incontinence:
Pregnancy and childbirth stretch pelvic tissues and nerves
Menopause reduces estrogen, affecting urethral support
Genetics influence connective tissue strength
Excess weight increases abdominal pressure
Chronic cough or heavy lifting compounds strain
Previous surgery can disrupt normal function
Remember: This isn't a personal failing—it's a mechanical issue with proven solutions.
Start with the Basics
Simple lifestyle changes can dramatically reduce symptoms:
Track Your Patterns
Keep a bladder diary for 3-7 days
Record fluid intake, bathroom visits, and leaks
This helps identify triggers and patterns
Optimize Your Habits
Fluid intake: Aim for 1.5-2 liters daily
Reduce caffeine and fizzy drinks if urgency dominates
Manage weight: Even 5-10% reduction helps stress leakage
Treat constipation: Reduces straining pressure
Stop smoking: Less coughing means fewer leaks
Master Pelvic Floor Training
This is the cornerstone of treatment for stress incontinence:
Work with a women's health physiotherapist
Learn proper technique (many women unknowingly use wrong muscles)
Expect 12-16 weeks of consistent training
Use apps or biofeedback devices for motivation
Maintain exercises long-term for lasting results
When to See a Specialist
Consult a urologist if you experience:
Ongoing leakage despite proper physiotherapy
Sudden urgency with pain or blood in urine
Recurrent urinary infections
Vaginal heaviness or visible prolapse
Persistent leakage 3-6 months after childbirth
History of pelvic surgery or radiotherapy
The Mesh Controversy: What You Need to Know
Mid-urethral mesh slings revolutionized incontinence surgery but came with risks:
The Reality:
Many women had excellent results and remain satisfied
Some experienced serious complications including pain and erosion
This led to increased scrutiny and demand for mesh-free options
Today's Approach:
Better consent processes and follow-up care
Multiple non-mesh alternatives available
Careful patient selection and outcome tracking
Modern Non-Mesh Treatment Options
Robotic Assisted Colposuspension
This cutting-edge procedure offers the precision of robotic surgery without synthetic mesh.
✅ No synthetic mesh
✅ Keyhole surgery
✅ 70-90% long-term success
✅ Quick recovery
How It Works:
Uses sutures to lift and support the urethra
Performed through small keyhole incisions
3D visualization allows precise suture placement
Creates a supportive "hammock" effect
Key Benefits:
No synthetic materials
Minimal scarring
Quick recovery (often overnight stay)
Excellent long-term results (70-90% success at 5-10 years)
Best For:
Stress-dominant symptoms
Women preferring mesh-free solutions
Can combine with prolapse repair
Recovery Timeline:
Light activities: 1-2 weeks
Full recovery: 6 weeks
Avoid heavy lifting during healing
Other Non-Mesh Options
Autologous Fascial Sling
Uses your own tissue to create support
Excellent for severe cases
Longer recovery but very durable
Urethral Bulking Injections
Minimally invasive day procedure
Good for mild-moderate symptoms
Quick recovery but may need repeat treatments
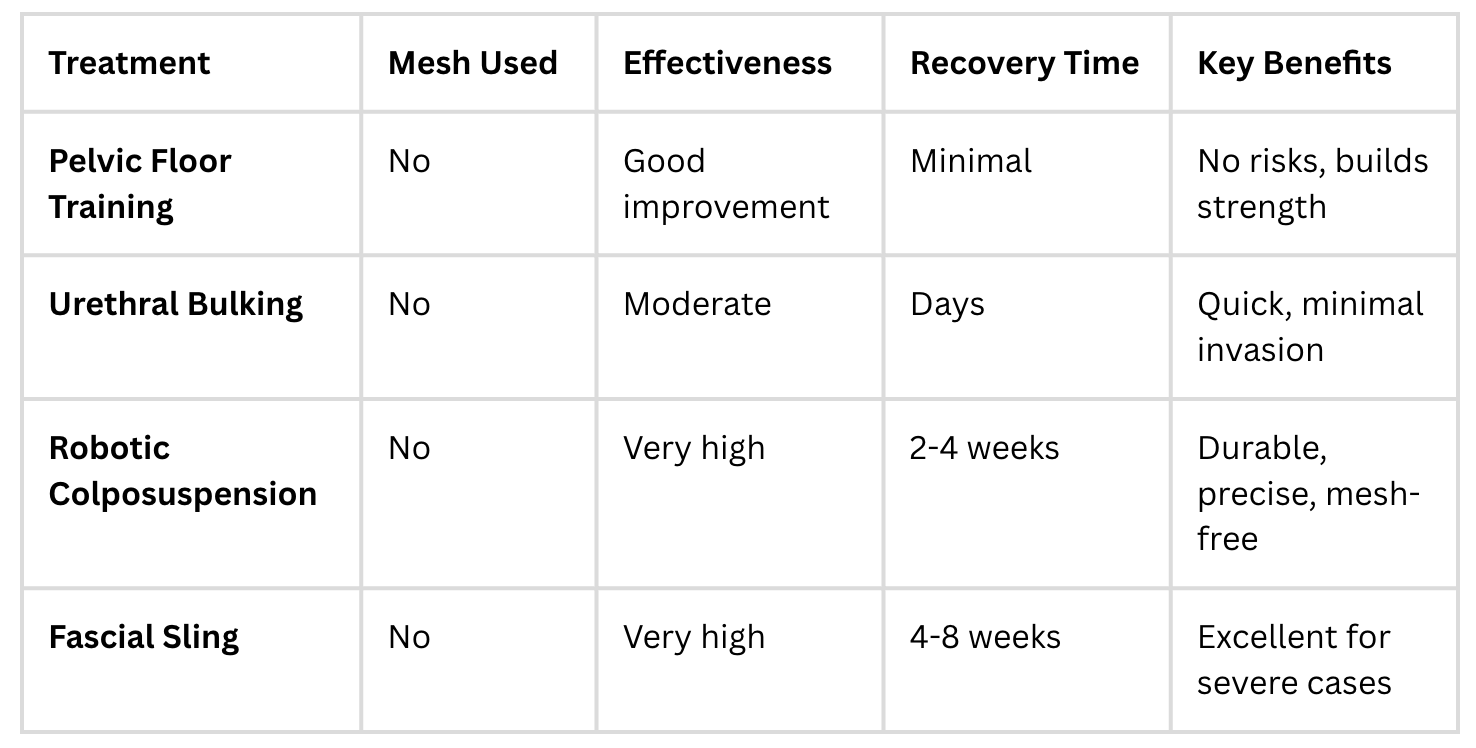
Treatment Comparison at a glance
Managing Urgency Symptoms
When urgency dominates, focus on bladder calming:
Bladder training with specialist guidance
Medications (antimuscarinics or beta-3 agonists)
Vaginal estrogen for postmenopausal women
Botulinum toxin injections for severe cases
Neuromodulation techniques for severe symptoms
What Modern Care Looks Like
Today's streamlined approach includes:
Comprehensive assessment
Shared decision-making with clear risk/benefit discussions
Prehabilitation with lifestyle optimization
Day-case procedures when possible
Digital follow-up and outcome tracking
Lifestyle Strategies That Work
Small changes make a big difference:
Space fluids throughout the day—sip, don't gulp
Limit caffeine after mid-afternoon
Schedule bathroom breaks to avoid rushing
Practice urge suppression: stop, squeeze pelvic floor, breathe, then walk calmly
Choose supportive exercise: walking, cycling, Pilates, swimming
Use proper incontinence products designed for urine
Debunking Common Myths
❌ "Leakage after childbirth is normal and untreatable"
✅ Reality: Effective treatments exist and work well
❌ "You can't return to high-impact sports"
✅ Reality: Many women resume full activities after proper treatment
❌ "Surgery means you don't need pelvic floor exercises"
✅ Reality: Ongoing muscle training supports any repair
The Bottom Line
Modern incontinence care is personalized, effective, and recovery-friendly. Many women improve significantly with physiotherapy and lifestyle changes alone. For those needing surgery, excellent mesh-free options like robotic colposuspension offer durable results with minimal disruption to daily life.
Don't suffer in silence. Start with a bladder diary and skilled physiotherapist, then seek a specialist who offers comprehensive options and transparent outcome tracking. With the right approach, you can reclaim confidence and get back to living life fully.